In the past, I’ve had conversations with colleagues about wellness initiatives. Instead of meeting general agreement or disagreement about my view on the topic, I’ve been shocked – on more than one occasion – that some people don’t care about wellness at all. They think wellness initiatives are soft and unnecessary.
This really got my gears churning.
See, I care very deeply about wellness in the medical community. It is an important and too infrequently discussed topic. Too many of our doctors are on the road to burnout. I want to be a part of the solution to that problem.
This does beg the question, though. Why do some people feel like physician wellness is a soft and unnecessary topic? Why are they inclined to think that discussing burnout isn’t important?
Today, I’ll give you three reasons why people don’t care about wellness. Then, I’ll respond to each position and show why these arguments don’t hold water.
Reason #1: Generational Differences
I am not quite sure where I fit in the whole generation discussion.
My place is somewhere in between a Generation X’er (Gen X’s) and the Millennial generation. One article called the people in the years in which I was born Xennials. I like this because I feel that I can relate to both the generation before (GXs) and after me (Millennials).
Those in Gen X often complain about Millennial “entitlement”. They bemoan the participation trophies the millennials demand, yet spend little time asking which generation provided the participation trophies in the first place (hint: It wasn’t the millennials).
The distinct differences between these two generations places wellness conversations in a very awkward position.
Gen Xer’s often describe their walk up hill both ways in snow when no one cared what they thought, felt, or did so long as it didn’t impact their jobs. [“See one, do one, teach one.” That’s safe, right?].
Because of their perception of how difficult training was in their time, they feel it unnecessary to discuss how “challenging” or “difficult” training is today. They see it as being vastly easier in comparison to their own experience.
Critique #1: Your Generation Isn’t Always Right!
Why do we need to make sure that residents are not burnout out? After all, the older attending “restrospectiscope” shows that they had it much harder than the current generation. These residents should just stop complaining!
There are many reasons that this line of thinking is flawed. Let’s touch on a few of them:
I’ll spare you the boredom of discussing all of the different memory biases that exist. Suffice it to say that just because someone remembers their experience one way doesn’t mean it is an accurate description or memory.
The previously mentioned “retrospectiscope” is not a valid instrument. We are all extremely biased when we look back on our past experiences.
We tend to remember things differently than they actually occurred.
Critique #2: Why would we NOT want to help?
Second, regardless of whether Gen X’s memories are accurate, it doesn’t change the question of whether we should help our trainees experience exceptional training at the same time that we help them deal with life issues.
The difficulties found in residency training are not unique to training. As we have discussed at length before, rates of depression and physician suicide are not unique to residents (though suicide is the number 2 overall cause of deaths during residency).
If we do not teach our trainees how to deal with life and residency difficulties now, they will not have the requisite skills to help them deal with this in their future practice in medicine.
A doctor a day kills themselves. Wrap your mind around that.
We need to stop pretending this isn’t a problem. Instead, we need to be a part of the solution to this burnout epidemic.
Critique #3: It isn’t always about the job!
The wrong question is being implied: “How do we help residents deal with a challenging residency?“
More often than not, its not the residency that is causing burnout or depression.
It is usually a combination of what we see in residency that is never discussed/processed in a formal way (pediatric deaths, traumatic events, untoward side effects, bad family discussions around death, etc) and other life events (marital stress, problems with kids, financial stress, etc).
Wellness has little to do with making residency “easier” and much more to do with helping residents experience, discuss, and process difficult life happenings.
We also must not forget that people have lives outside the hospital. Divorces happen. Friends and family die. A struggling resident is not a weak resident. They are a resident in need.
Reason Number 2: Show me the Money
We have looked into the financial aspect of attacking wellness before. So, I’ll keep this short. Simply put, administrators love metrics. They tend to be “bean counters.”
If you can’t show them numbers that will change their bottom line, very rarely do they care. This makes wellness a difficult problem to tackle. Until recently, the financial aspect of burnout has been difficult to measure and quantify.
More difficult still is is figuring out a way to measure the impact of changes on wellness and whether they produce an adequate return on investments.
Critique: I’ll show you the money
The post linked above goes into a lot of the detail needed to have this conversation. I’ll let what I said their speak for itself. However, I will add one thing:
There is one aspect of wellness that is free of charge to training programs: Wise Teachers.
If those supervising young trainees would take the time to debrief following a potentially traumatic experience, this could prove really helpful teaching the trainee how to process difficult situations.
Simply saying, “That’s tough. Are you handling that okay?” is enough to have a good conversation. It takes little time, costs nothing, and really helps.
These same faculty could stop making excuses and teach residents about personal finances, which plays a large part in their picture of stress.
Reason Number 3: The Stigma
Unfortunately, there is a stigma involving mental health, burnout, and depression. The stigma doesn’t stop with our patients.
This stigma also exists in the medical community.
It is common to think less of those that are struggling with these issues and to view them as a “lesser” person. They simply must not be “tough enough.”
As humans, we (unfortunately) rarely want to help people we think less of or look down on. So, starting a wellness initiative to help others we think just need to “fix things” is unlikely. Surely, you’ve heard of someone saying something like “they just need to pick themselves up by the boot straps!”
The fact that the brain is viewed this way is baffling to me. If you have severe kidney disease because you were born with polycistic kidneys, we feel bad for you. If you were born with cystic fibrosis and have trouble breathing, we feel bad for you.
But if you were born with a predilection towards mental illness, there is something wrong with you. You are weak!
I find this double standard absurd as we now know that many of these diseases are related to altered levels of neurotransmitters in our brain or even structural changes (think about chronic traumatic encephalopathy often discussed in the NFL).
Critique: The Brain is an Organ, Too
Mental health problems can be treated just like the patient with coronary artery disease or high cholesterol.
One of the first ways we can help this is by not being part of the stigma and being part of the community that cares and is on board with putting resources into helping our colleagues.
Take Home
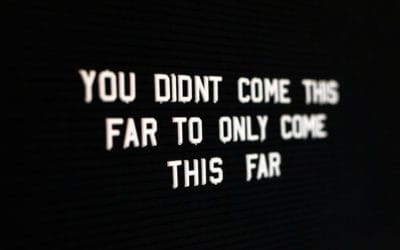
All of us need to stop making excuses about the physician burnout problems that exist in our country. Instead, we need to be a part of the solution.
Do you think wellness initiatives are a waste of time and money? Have you been helped by a wellness program? Is this something that we, as a medical community, should invest in?
TPP





0 Comments